Health professionals providing care for a patient following a sexual assault
The Sexual Assault Resource Centre (SARC) provides crisis services, support and information to people who have experienced a recent sexual assault in the last two weeks and counselling for sexual assault / abuse experienced recently or in the past.
SARC Kits for early response to sexual assault have now been launched across WA and have replaced the previous version of the Early Evidence Kit (EEK). To support health care workers in using the new kits, a comprehensive SARC eLearning is now available.
To access the Early Response to Sexual Assault in WA eLearning package:
- WA Health employees: access through MyLearning (external site) search the catalogue for "SARC".
Videos and supporting documents are also available on the staff SARC Education SharePoint (external site). - Private WA Hospitals please contact your Education and Training department for access.
- Aboriginal Medical Services sites and other organisations who stock Early Evidence Kits please complete a form (external site) to receive a password.
- Mining industry: access to the eLearning is now available.
Who can be referred to SARC
Perth metro area
- Patients can be referred though hospitals, GPs, police and other health or social services. Patients are also able to self-refer.
- SARC see people of all genders aged 13 years and over for medical and/or forensic assessment.
- The SARC medical forensic team will see patients up to 2 weeks after a sexual assault.
- SARC can see people whether or not they intend reporting to police.
- SARC doctors may refer a patient to ED if SARC suspects a serious injury, acute psychiatric illness or intoxication which cannot be safely managed at SARC.
- SARC can see people who don't hold a Medicare card and can also see people no matter their visa status.
- Crisis services for people under 13 years are provided by the Child Protection Unit (external site) at Perth Children's Hospital. They can be contacted by calling (08) 6456 0089.
Regional and remote – WACHS
- SARC doctors are on-call 24 hours a day for state-wide telephone advice to health professionals who are seeing patients alleging a recent sexual assault. This service is available to staff in all regional rural and remote areas. Health professionals are encouraged to contact SARC when seeing patients reporting recent sexual assault.
- SARC doctors provide specific specialist advice to health professionals who have been asked to perform forensic specimen collection by the police.
Mining Industry
- Use the steps for responding to sexual assault (PDF) for mining and contact SARC on 6458 1828.
How to refer a patient to SARC
The SARC Duty Doctor can be directly contacted at SARC (08) 6458 1828 in hours or via KEMH switchboard (08) 6458 2222 out of hours.
The patient will be required to speak directly to a SARC counsellor for triage purposes. SARC is a voluntary service and the patient must understand and consent to being seen by SARC workers. The outcome of the triage will be communicated back to the referring healthcare professional.
WA Health emergency departments and AMS
To assist you in your SARC referral please use the Sexual Assault Checklist (PDF) found in the First Response Pack when referring patients to SARC.
Mining Industry
Use the steps for responding to sexual assault (PDF) for mining and contact SARC on 6458 1828.
Serious injury
If a patient has serious injuries, they should be triaged and treated medically as per the protocol of your department/organisation. Medical concerns take priority over forensic issues.
- Assess and treat intoxication, poisoning, injuries and psychiatric emergencies as you would any other patient. Assess injuries specific to penetration, such as vaginal or anal pain or bleeding and abdominal pain.
- Ask about non-fatal strangulation (PDF) and assess for complications.
- If serious injuries are suspected, consider the need for surgical or gynaecological referral.
- Unless it's an emergency or the patient declines a forensic examination, discuss any internal examination with the SARC doctor before proceeding as this can impact forensic evidence collection. Always include the SARC doctor when planning surgical or gynaecological referrals so appropriate forensic examinations can be arranged.
- Further training on non-fatal strangulation is available on the medical education page.
Medical and safety considerations following a sexual assault
Consider:
- Emergency contraception: Ulipristal (EllaOne) can be taken up to 120 hours and levonorgestrel (LNG) can be taken up to 96 hours after unprotected sex. Ulipristal is more effective. Both are available over the counter. A Arrange a pregnancy test three weeks post assault if relevant.
- STI and blood-borne virus investigations and prophylaxis. Discuss with the SARC duty doctor first, especially if the patient is considering a forensic examination.
- Advise patient to have a repeat sexual health screen at 2 to 4 weeks and repeat a blood borne virus serology and syphilis screen at 3 months, if relevant. Promote safe sex practises.
- Complete a mandatory report if required.
- Assess ongoing risk. Ensure the patient has a safe place to return to and psychological support has been organised as needed.
- Provide the patient with the patient information leaflet from the First Response Pack and ensure the patient is aware how to contact SARC.
SARC have produced a guide to assist GPs (PDF) in the management of patients after sexual assault.
SARC kits
SARC have developed three kits to help professionals in responding to a disclosure of sexual assault.
To support health care workers in using the kits, a comprehensive SARC eLearning is now available.
To access the Early Response to Sexual Assault in WA eLearning package:
- WA Health employees: access through MyLearning (external site) search the catalogue for "SARC".
Videos and supporting documents are also available on the staff SARC Education SharePoint (external site). - Private WA Hospitals please contact your Education and Training department for access.
- Aboriginal Medical Services sites and other organisations who stock Early Evidence Kits please complete a form (external site) to receive a password.
- Mining industry: access to the eLearning is now available
First Response Pack
- Designed to assist those in responding to disclosure of sexual assault
- There are two different types of first response pack. One for use in emergency departments and AMS and one for use in the mining industry.
Emergency departments and AMS
- Contains Sexual Assault Checklist (PDF) to help guide relevant history taking
- Patient information leaflet (PDF) which should be provided to the patient
Mining Industry
- Contains Steps for responding to sexual assault (PDF)
- Patient information leaflet (PDF) which should be provided to the patient
Early Evidence Kits
An Early Evidence Kit (EEK) is used to collect time-sensitive forensic specimens before a full forensic examination can be arranged.
Forensic Toxicology Kits
A Forensic Toxicology Kit is used to collect time sensitive forensic toxicology specimens. If a person is intoxicated from medications, illicit drugs or alcohol they may have been unable to consent to sexual activity.
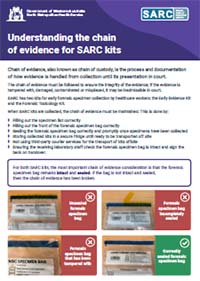
Understanding the chain of evidence for SARC Kits
It is essential that the chain of evidence of forensic specimens is maintained throughout collection and transport. The PDF document below provides further guidance regarding this:
For GPs (metro and rural)
SARC encourage all WA GPs to discuss patients who disclosure of recent sexual assault with SARC.
The SARC Duty Doctor can be directly contacted at SARC (08) 6458 1828 or via KEMH switchboard (08) 6458 2222.
- SARC encourages GPs to use the Sexual assault checklist (PDF) when responding to sexual assault.
- A patient information leaflet (PDF) is available for download. GPs are encouraged to provide a copy to patients who disclose a recent sexual assault.
- Useful information on responding to sexual assault as a GP (PDF), including information on STI testing and further support.
- Information on what a full forensic examination entail (PDF)
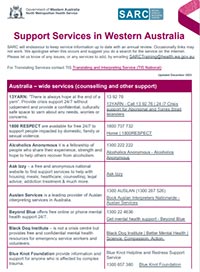
- A list of support services in WA (PDF)
Counselling Services at SARC
SARC offers two types of counselling services:
- Crisis telephone counselling for people in emotional crisis from an unwanted sexual experience (recently or in the past).
The service can be accessed by calling (08) 6458 1828 or 1800 199 888 (freecall from landlines) between 8:30am and 11pm, any day of the week. Clients do not need to provide their full name if they do not wish to. - Face-to-face counselling for any sexual assault / abuse experienced recently or in the past.
Patients can call to request an appointment on (08) 6458 1828 between 8.30am to 4.30pm, Monday to Friday. Please note SARC is currently experiencing long wait times for face-to-face counselling services.
More information about SARC counselling services.
SARC does not provide services to perpetrators of sexual abuse or sexual assault.
Information and resources
Open resources page.