Pharmacy
We provide medicines and medicines information to patients, carers and other healthcare professionals in a timely manner.
Pharmacy is dedicated to providing quality use of medicines via the following services:
- Outpatient pharmacy service.
- Medicines information including: medicine specific genetic counselling and publications.
- In-patient and clinical pharmacy service.
- Quality use of medicines including adverse drug reaction reporting and antimicrobial stewardship.
- Research, teaching and clinical trials services.
Pharmacy Outpatient Services
The outpatient pharmacy is located on the lower ground floor of the main hospital, most accessible from Hensman Road. The Pharmacy is open from 8:30am to 5pm Monday to Friday.
Medication during my hospital stay
It is important for your medical team to know exactly what medicines you are taking in case they interact with medicines used in hospital.
Pharmacy can provide written information to patients, such as consumer medicine information leaflets and discharge medicines lists.
If you have any concerns or have experienced any unexpected or troublesome side effects from your medicines, let your pharmacist, nurse or doctor know.
If you require any medicines on discharge, you will receive a prescription and can purchase your medication at the hospital pharmacy or your local community pharmacy. Your ward pharmacist will be able to discuss your medicines in more detail as part of your hospital discharge.
What to bring
- Your medications.
- Your Medicare card.
- Your Health Care Card, Pension card or safety net card (if you have one).
Cost of Medications
You will be charged a contribution fee for all medicines that are dispensed from our pharmacy at discharge or as an outpatient. The amount of the patient contribution fee is determined by commonwealth and state regulations and adjusted every year on 1st January in line with the consumer price index (CPI).
If you choose to get your medications from the hospital, you will get a payment advice which you can pay on the day of discharge with cash, EFTPOS, MasterCard, Visa or cheque or an invoice will be posted to your home.
If you believe you may experience difficulty in paying for your prescribed discharge medications please talk to your nurse, midwife, doctor or the KEMH Social Work department during your stay in hospital.
Cashier
Opening hours: 8:45am to 4:45pm, Monday to Friday (closed weekends and public holidays).
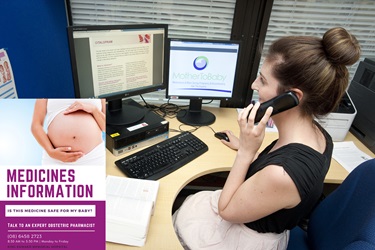
Medicine Information line
The Obstetric Medicines Information Service at WNHS provides mothers, families and health professionals information about the safe use of medicines during pregnancy and when breastfeeding.
The Medication Safety Line is available on (08) 6458 2723 and provides information to women anywhere across Western Australia between 8.30am and 4.30pm Monday to Friday. Women, unsure of the effects of medication either prescribed or over the counter, can call to receive reassurance from qualified Pharmacists.
Often uncertain about the safety of taking medications during pregnancy and breastfeeding, the line provides an enormously valuable resource for WA Women.
Medicines information in pregnancy and breastfeeding - helpline (PDF)
Medicines in pregnancy
Many women need to take medicines during pregnancy for either new or ongoing conditions that require treatment. Every pregnancy begins with a 3 to 5 percent chance of developing a birth defect, which is called the ‘background risk’. Medicine exposure accounts for only a small proportion of these birth defects.
Pregnancy can also impact the way that the body processes medicines, which can lead to changes in the amount of medicine you need. It is important to consider the risks and benefits of treating a condition with medicine versus the potential effects of that medicine on the pregnancy.
It is recommended that medicines are used at the lowest effective dose for the shortest possible duration.
The impact of medicine on the fetus can vary throughout the pregnancy, depending on the period it is taken. In very early pregnancy, a harmful exposure is most likely to cause an ‘all or nothing’ response - meaning that it may either cause a miscarriage or not have a significant effect on the pregnancy. During the first trimester, harmful exposures are most likely to cause birth defects because this is when major structural formation occurs. In the second and third trimester, harmful exposures are more likely to cause growth problems, preterm birth and newborn withdrawal symptoms.
Important information
It is important that all decisions relating to medicine use in pregnancy are made with your healthcare providers. Before starting, continuing, changing or stopping a medicine during pregnancy, it should be discussed with a doctor, pharmacist and / or midwife.
Commonly used medication
Hay fever and allergies
Hay fever symptoms include a runny or blocked nose, sneezing, itching of the eyes or nose and watery, irritated eyes. Avoiding or limiting exposure to substances that cause hay fever, such as pollens, house dust mites and animal dander, can help reduce symptoms.
Simple measures such as saline nasal sprays can assist in removing allergens from the nasal passages.
Oral and nasal antihistamines
Antihistamines reduce the symptoms of hay fever but don’t always help nasal congestion. There is more safety information about the older oral sedating antihistamines, such as promethazine and dexchlorpheniramine, and they may be used at recommended doses at any stage in pregnancy. Less sedating oral antihistamines, such as loratadine, are also considered safe to use in pregnancy at recommended doses.
Antihistamine nasal sprays and eye drops containing azelastine, levocabastine and ketotifen (eye preparation only) can be used when needed to relieve symptoms of hay fever and are safe to use in pregnancy. They generally start to work quickly after use (usually within 15 minutes). When using eye drops, apply pressure against the inner corner of the eye for one to two minutes and blot away any excess drops to help minimise absorption into your system.
Corticosteroid nasal sprays containing budesonide and mometasone can give some symptom relief by reducing inflammation in the nose. Because these medications act locally at the nose and are likely to enter the mother’s bloodstream in very small amounts only, they are considered safe in pregnancy.
Decongestant nasal sprays (see cold and flu) may be used short term if corticosteroid and antihistamine nasal sprays have not relieved the symptoms.
Aches and pains
Paracetamol is considered safe to use in pregnancy and is effective in treating aches, pains and fever. It is important that no more than 8 tablets (containing 500mg of paracetamol) are taken within a 24-hour period.
Anti-inflammatory medicines - including topical preparations e.g., creams are NOT recommended in pregnancy (especially in the third trimester).
If paracetamol is inadequate or unsuitable, short-term use of some opioid medicines to treat moderate to severe pain is considered safe to use in pregnancy. Regular use of these medicines late in pregnancy can cause newborn withdrawal symptoms, so it is important to inform your healthcare providers of their use. These medicines can also lead to dependency and, if used consistently, can become less effective. It is necessary to consult your doctor if opioid pain relief is required.
Cold and flu
Common colds are caused by a virus and often include symptoms such as sore throat, cough, runny and / or blocked nose, sneezing, body aches, mild headache and general tiredness. Colds typically resolve on their own and usually only require treatment for individually bothersome symptoms.
Sore throat
A sore throat can be relieved by drinking warm lemon and honey drinks or gargling warm, salty water. Lozenges containing antibacterial and anaesthetic (numbing) agents are considered safe to use in pregnancy at recommended dosages. Medicines containing benzydamine (anti-inflammatory) should not be used in pregnancy unless under the direction of a doctor. Gargles containing povidone-iodine should be avoided as there is a risk that it may affect the thyroid of the developing fetus.
Cough
For a dry, tickly cough, dextromethorphan is considered safe to use in pregnancy. It provides relief by suppressing the cough while the immune system recovers from the virus.
For a chesty, productive cough, medicines such as bromhexine and guaifenesin are considered safe to use in pregnancy. They provide relief by facilitating the removal of mucus from the chest.
Runny or blocked nose
A runny nose can be treated with oral sedating antihistamine medicines (see hay fever and allergies). A blocked nose can be treated with decongestant nasal sprays (oxymetazoline or xylometazoline), saline nasal sprays or steam inhalation. Very small amounts of these medicines are expected to absorb into the body from nasal sprays, therefore, they are considered safe to use in pregnancy. Decongestant nasal sprays should not be used for more than three days at a time due to the risk of rebound congestion. Oral medicines to treat a blocked nose, such as pseudoephedrine or phenylephrine, are not recommended in pregnancy.
Constipation
Constipation is very common in pregnancy and eating high-fibre foods, such as wholegrain cereals and bread, fresh fruits and vegetables, along with drinking plenty of fluids, regularly exercising and going to the toilet as soon as you feel the urge, help to maintain regular bowel motions in pregnancy.
Fibre supplements (bulk-forming laxatives) such as psyllium, sterculia and ispaghula are suitable to use with plenty of water. Osmotic laxatives such as macrogol, lactulose and sorbitol draw water into the bowel and help to soften the stool. A stool softener such as docusate is also safe to use in pregnancy but the use of stimulant laxatives such as senna and bisacodyl are not recommended for regular use.
Medicines taken in pregnancy such as antacids for heartburn, strong pain medicines, multivitamins, iron and calcium tablets, or nausea and vomiting can make constipation worse.
Reflux / heartburn
Heartburn can develop in up to 80 percent of pregnant women. In late pregnancy, this is made worse by the increasing pressure of the baby on the stomach. Dietary and lifestyle measures, such as eating smaller, more frequent, meals; avoiding spicy and highly fatty foods; not lying down immediately after a meal or eating late at night, may help to reduce symptoms.
If these measures are not working, then oral liquid antacids (eg: Gaviscon®, Gastrogel®) can be tried at the recommended dosages. A group of medicines called H2 Antagonists (eg: Famotidine) are considered safe to use in pregnancy if antacids are ineffective. Another group of medicines called proton pump inhibitors (PPIs), such as omeprazole, may be considered for use.
Haemorrhoids
Haemorrhoids are swollen and enlarged veins in the anus and rectum that can be either internal, external or a combination of the two. They are common in pregnancy and can be triggered by pressure from the uterus, hormone changes and constipation. The best way to manage haemorrhoids is with lifestyle modifications such as:
- Taking a warm bath
- Applying ice packs to external haemorrhoids to reduce pain and swelling
- Ensuring adequate fibre and fluid intake (see constipation above)
- Trying not to strain during bowel movements and going to the toilet when the urge is felt
In some cases, haemorrhoids can cause discomfort that interferes with quality of life. In these circumstances, they can be treated with suppositories/ointments containing an anaesthetic and/or steroid (eg:. Proctosedyl®, Rectinol®), which are considered safe to use in pregnancy. These can be used up to three times a day and are best applied after a bowel motion - for no longer than seven days.
Vaginal thrush
Vaginal thrush is one of the most common fungal infections during pregnancy. Typical symptoms include itching, stinging, burning, and a thick, white, vaginal discharge.
Vaginal antifungal creams and pessaries containing clotrimazole or nystatin are considered safe during pregnancy and are the treatments of choice. Vaginal applicators may be used with care in pregnancy.
At least a six-day course of clotrimazole or a 14-day course of nystatin is recommended in pregnancy, rather than a shorter course.
A single dose of oral fluconazole is not routinely recommended during pregnancy unless it is advised by your doctor.
Cold sores
Cold sores occur commonly during pregnancy and are not thought to affect the unborn baby. Ice is a recommended treatment for cold sores and can be applied to the affected area.
Antiviral medicines such as aciclovir cream can be used safely at all stages of pregnancy. If the cold sores are severe, an oral course of aciclovir or valaciclovir from your doctor would be considered safe to use at all stages of pregnancy.
Avoiding triggers such as sun and wind exposure, stress, or certain food and drinks can reduce the likelihood of an outbreak. Using lip balms with SPF15+ can also minimise your risk of cold sores.
Nausea and vomiting
See Nausea and vomiting in pregnancy (PDF)
Herbals
There is very little information available on the safety of herbal preparations in pregnancy, or their effect on your baby. Care should be exercised with their use. Talk to your doctor or pharmacist to discuss your options and for further advice.
Vitamins
Having a well-balanced, healthy diet is important during pregnancy to ensure you and your baby’s needs are met. Vitamins such as folic acid, iron, vitamin D and iodine are especially important during your pregnancy. For more information see Chapter 3 ‘Taking care of yourself’ Pregnancy, birth and your baby (PDF).
COVID-19 and flu vaccine
The Comirnaty Pfizer®, SpikeVax Moderna®, Nuvaxovid NovaVax® and annual influenza vaccines are considered safe in pregnancy. These vaccines are recommended for women who are pregnant.
References
Medicines and breastfeeding
The importance of breastfeeding is well recognised with benefits for both the mother and infant. Breast milk provides babies with unique nutrients that are ideal for their immune protection, growth and development.
Many breastfeeding mothers need to be treated with medicines, either for a chronic illness requiring ongoing therapy or for an acute illness requiring only a few days therapy. Some mothers stop breastfeeding while taking medications to treat these conditions because of unfounded concern or inappropriate advice.
It is widely accepted that medications transfer into human milk to some degree, although the amount is generally quite low and this is why most medicines are considered safe to take while breastfeeding. Only rarely does the amount transferred into breastmilk produce clinically relevant doses in the infant.
The safety of breastfeeding while a mother is taking a medication may be assessed by weighing the risks of potential adverse effects in the baby, against the benefits of the medicine for the mother and the benefits of breastfeeding for the baby and mother.
Minimising transfer of medications into breastmilk
- Avoid using medicines unless they are necessary.
- Your doctor will prescribe the lowest dose for your condition.
- Think of ways to choose a dose that reduces how much is passed into breastmilk e.g. use a decongestant nasal spray rather than an oral decongestant.
- To reduce the amount of medicine in the breastmilk, time your feed eg. taking a dose immediately after a feed, or before baby’s longest sleep period.
Important information
When taking any medicine, watch for signs of possible side effects in your baby such as increased sleepiness, poor feeding, rash and severe diarrhoea.
If these are troublesome and continued, contact your doctor
Always ask your pharmacist what is in a medicine and tell them you are breastfeeding.
Commonly used medications
Aches and pain - analgesics
- Non-steroidal anti-inflammatory medicines (NSAIDs) like ibuprofen or diclofenac have low transfer to breast milk and are considered safe to use to relieve pain and inflammation.
- Paracetamol can be used safely during breastfeeding to treat mild pain or reduce fever.
- Low doses of aspirin, less than 150mg daily, are considered safe to take. Larger doses should be avoided as they may be harmful to your breastfed infant.
- Medications containing codeine
Medications containing codeine are no longer recommended for pain relief in breastfeeding mothers.
Codeine metabolises to morphine in the body and a small number of people produce higher than expected morphine levels in their blood resulting in an increased risk of transfer to the infant via the breastmilk. Alternative pain control medicines as mentioned above are recommended.
Cold and flu
Body aches and pain – see above (analgesics)
Nasal symptoms
- Steams inhalations and saline (sodium chloride) nasal spray may be used to relieve a blocked nose while breastfeeding.
- Decongestant nasal sprays (oxymetazoline, xylometazoline) may be used for 3 to 5 days.
- Avoid oral preparations containing pseudoephedrine as it may reduce milk production or cause irritability in a breastfed baby.
Cough
- A cough is usually self-limiting. If treatment is required, use guaifenesin, bromhexine or senega and ammonia mixture for a chesty cough.
- A cough suppressant like dextromethorphan is considered safe for a dry cough. Avoid combination preparations containing pseudoephedrine and phenylephrine – always ask your pharmacist what is in a medicine.
Sore throat
- Lozenges or throat gargles containing local anaesthetic, antibacterial agents or benzydamine may be used while breastfeeding.
- Avoid products containing povidone-iodine (e.g. Betadine®) as it may affect the thyroid function of your baby.
Allergies and hay fever - antihistamines
- Non-drowsy antihistamines such as loratadine, desloratadine and fexofenadine are present in very small amounts in breastmilk and are considered safe to use whilst breastfeeding. Drowsy antihistamines such as cetirizine, dexchlorpheniramine or diphenhydramine may make your baby drowsy, so less sedating antihistamines are preferred.
- Nasal sprays containing beclomethasone, fluticasone or budesonide may be used while breastfeeding. Topical eyedrops for allergies and hay fever may be used as the amount transferred into breastmilk is low. Eye drops containing antazoline and naphazoline are considered safe to use.
Anti-infectives
Which antibiotics are safe?
Most antibiotics transfer into breastmilk, but the amount ingested by an infant is unlikely to cause serious harmful effects. However some antibiotics can cause changes in gut bacteria and infants should be observed for adverse effects such as diarrhoea, vomiting, skin rashes or thrush.
Penicillin antibiotics (including amoxicillin, amoxicillin with clavulanate and flucloxacillin), cefalexin, erythromycin and azithromycin are considered safe. Metronidazole is considered safe in doses up to 400mg three times a day, although it may give the milk a bitter taste.
What can I use to treat worm infections?
Both pyrantel and mebendazole are considered safe as they are poorly absorbed from the gut and are unlikely to be passed into breast milk in clinically relevant amounts.
What can I use for vaginal thrush?
Topical antifungal cream and pessaries containing clotrimazole, miconazole and nystatin are safe to use while breastfeeding.
A single dose of oral fluconazole is considered safe to use whilst breastfeeding.
What can be used to treat cold sores?
Ice is a recommended treatment which can be applied to the affected area.
Antiviral medicines such as aciclovir cream can be used in breastfeeding, and if the cold sores are severe an oral course of aciclovir or valaciclovir from your doctor would be considered safe to use whilst breastfeeding. These options are preferred to famciclovir which has no published data on how much enters breastmilk.
Head lice
Non-insecticidal treatment ─ 10 days hair conditioner method: Apply plenty of hair conditioner to the dry hair until saturated, use ordinary comb to remove tangles, then use metal fine tooth nit comb in 4 directions (forward, backward, left and right). Remove lice from comb. Rinse out and dry hair. Repeat every 1 to 2 days over a 10-day treatment period.
Insecticidal treatment – Permethrin, Dimeticone or pyrethrin / piperonyl butoxide can also be used if needed. Treatment should be repeated in 7 days to kill lice that have hatched.
Flu vaccine
Breastfeeding mothers may continue to breastfeed after immunisation with flu (influenza) vaccine.
COVID-19 vaccines
The Comirnaty Pfizer®, SpikeVax Moderna® and Nuvaxovid NovaVax® vaccines are considered safe to be used whilst breastfeeding. These vaccines are recommended for women who are breastfeeding. You can continue breastfeeding before or after your vaccination.
Antidepressants
Some antidepressants are considered compatible with breastfeeding. Talk to your doctor or pharmacist to discuss your options and for further advice.
Herbal preparations
There is very little information available on the distribution of herbal preparations into breast milk, or their effects on lactation. Care should be exercised with their use. Talk to your doctor or pharmacist to discuss your options and for further advice.
Oral contraceptives
The progesterone-only “minipill” is the preferred oral contraceptive for breastfeeding women as transfer to milk is minimal and lactation is not affected.
The combined estrogen-progesterone pill may decrease the quantity and alter the composition of breastmilk. It may be considered after 6 weeks if breastfeeding is well established.

